Journal highlights
The following are highlights from the current issues of RSNA’s peer-reviewed journals.
Intraarticular Steroid Injection in Hip and Knee with Fluoroscopic Guidance: Reassessing Safety
Intraarticular corticosteroid (IACS) injections are a frequently used therapy for hip and knee osteoarthritis (OA) and are recommended by more than two-thirds of OA organizations. However, there is conflicting data about the benefits and complications of IACS injections. Additionally, there is a lack of studies with radiographic follow up that provide data from before and after IACS injection. Thus, additional research is needed to clarify the complications of IACS injections and better identify the risk factors.
In a study published in Radiology, Dimitri Graf, MD, Balgrist University Hospital, Zurich, and colleagues determined the number of patients with complications after hip and knee IACS injections in a large study sample with long-term follow up. The authors analyzed the pre- and peri-interventional images, as well as the postinterventional images obtained with all available modalities (conventional radiography, fluoroscopy, CT and MRI). This study included 500 patients for the knee joint and 500 for the hip joint that were randomly picked between January 2016 and May 2020.
Of the 1,000 patients in this study, 10 developed severe complications: four with osteonecrosis, three with insufficiency fractures and three with rapid progressive OA. Of the 1,000 patients who received IACS injections, 10 individuals experienced adverse events within 12 months after injection. Ninety percent of these complications affected women.
“Intraarticular steroid injection is substantially safer than smaller studies have reported. However, the strong predominance of complications seen in women needs further evaluation,” the authors conclude.
To read the full article, go to RSNA.org/ Radiology. Follow the Radiology editor on Twitter @RadiologyEditor.
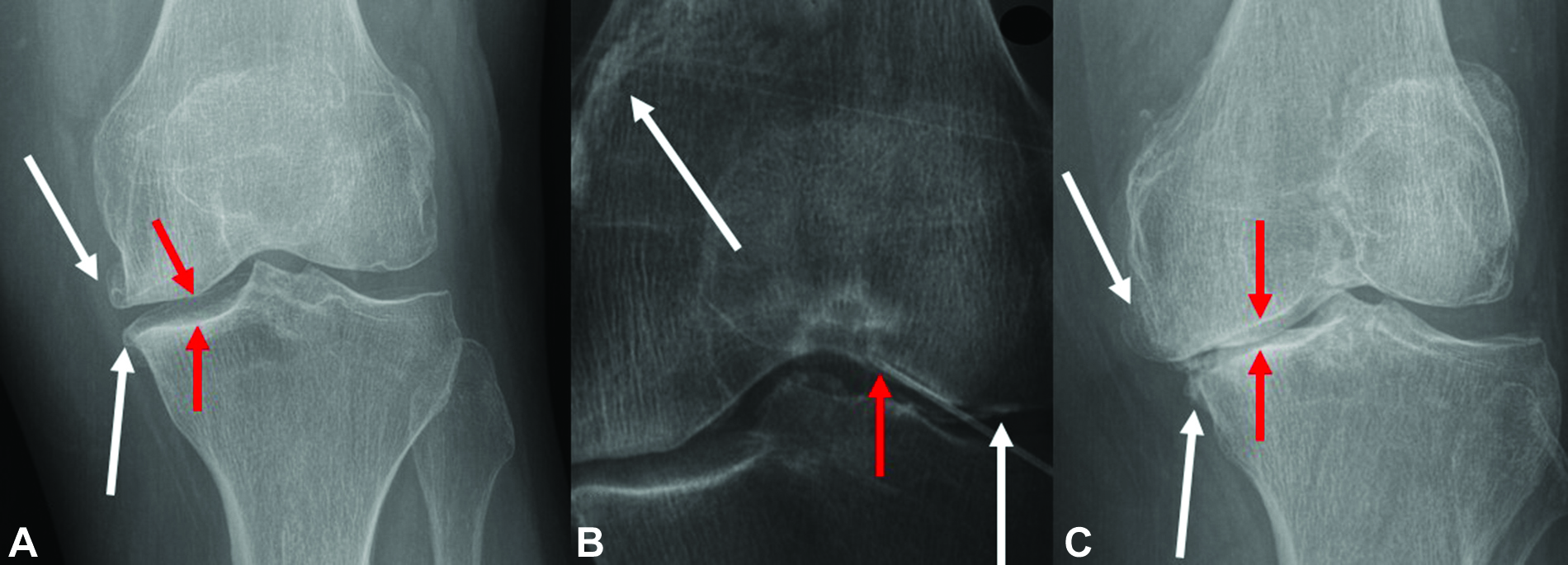
Rapid progressive osteoarthritis (RPOA) in an 82-year-old woman who presented with knee pain. (A) Anteroposterior left knee radiograph with joint space narrowing (red arrows) and osteophytes (white arrows). (B) Periprocedural fluoroscopic image with needle placement in the intercondylar notch (red arrow) with an anterolateral approach and contrast media in the suprapatellar recess and femorotibial joint space (white arrows). (C) Anteroposterior left knee radiograph obtained 4 months after the procedure with severe and progressive joint space narrowing (red arrows) and osteophytes (white arrows) after persisting symptoms.
https://pubs.rsna.org/doi/10.1148/radiol.210668 ©RSNA 2022Imaging Cancer in Pregnancy
Pregnancy-associated cancer (PAC) is defined as cancer that is detected during pregnancy and up to one year postpartum. Although rare, about 1 in 1,000 pregnancies, PAC is increasing because of postponed childbearing and advanced maternal age at conception.
Detection is based on signs and symptoms, results of laboratory analyses and incidental findings during routine obstetric imaging. The care of PAC necessitates balancing the potential benefits of diagnosis and treatment of the mother with risks to the fetus.
In an article published in RadioGraphics, Priyanka Jha, MBBS, Department of Radiology and Biomedical Imaging, University of California, San Francisco, and colleagues provide an update of the imaging triage, safety considerations, cancer-specific imaging and treatment options for cancer in pregnancy. According to the authors, the most common PACs are breast cancer (41%), lymphoma (12%), uterine cervical cancer (10%), leukemia (8%) and ovarian cancer (7%).
Because the benefits of timely imaging diagnosis of PACs must be weighed against related risks to the fetus and treatment-related fetal side effects, screening for PACs and congenital fetal anomalies is typically performed with US and noninvasive prenatal tests. However, the use of other modalities such as CT or nuclear medicine requires a careful assessment of risk versus benefit from radiation exposure.
“This updated review of diagnostic imaging of PAC emphasizes safe imaging triage, minimization of risk to mother and fetus while optimizing outcomes, integration of imaging into clinical decision making and malignancy-specific solutions for extent of disease and staging workups,” the authors note.
Read the full article and invited commentary at RSNA.org/RadioGraphics. This article is also available for CME at RSNA. org/Learning-Center. Follow the RadioGraphics editor on Twitter @RadG_Editor.
Lymphoma in pregnancy in a 32-year-old woman who presented with respiratory distress at 22 weeks gestational age. The imaging workup showed a mediastinal mass that at tissue sampling by US guidance was proven to be B-cell lymphoma. Staging noncontrast MR images (not shown) showed no additional sites of disease. Chemotherapy was started at 24 weeks GA. The patient presented with premature rupture of membranes and had an uncomplicated vaginal delivery at 35 weeks GA. (A) Axial contrast-enhanced CT image of the chest shows a large anterior mediastinal mass (arrows). (B) Gray-scale split-screen US image through the supraclavicular space shows the heterogeneous hypoechoic mass (*). The dotted lines on the right image show the expected path of the needle when using the US biopsy guide device. US can provide percutaneous access to sonographically accessible lesions to minimize exposure to ionizing radiation.
https://pubs.rsna.org/doi/10.1148/rg.220005 ©RSNA 2022
Fully Automated 3D Vestibular Schwannoma Segmentation with and without Gadolinium-based Contrast Material: A Multicenter, Multivendor Study
Vestibular schwannomas are rare, benign intracranial tumors arising from the neurilemma of the vestibular nerve. Initial symptoms usually involve hearing loss, tinnitus and balance disturbance.
While small- to medium-sized tumors are not life-threatening and are at least initially managed using surveillance with repeated MRI examinations, patients with large tumors at presentation, or tumors that progress during follow-up, may need radiation therapy or intervention. There are no reliable predictors for tumor progression.
In an article published in Radiology: Artificial Intelligence, Olaf M. Neve, MD, Leiden University Medical Center, the Netherlands, and colleagues sought to develop automated vestibular schwannoma measurements on contrast-enhanced T1- and T2-weighted MRI scans. They analyzed data from 214 patients in 37 different centers. After randomly assigning patients with hearing loss to training, validation and an independent test set, they trained the convolutional neural network (CNN) using fivefold cross-validation for two models, T1 and T2.
“The CNN model detected and delineated vestibular schwannomas accurately on contrast-enhanced T1- and T2-weighted MRI scans and distinguished the clinically relevant difference between intrameatal and extrameatal tumor parts,” the authors conclude.
To read the full article go to RSNA.org/AI. Follow the Radiology: Artificial Intelligence editor on Twitter @Radiology_AI.

Animal Models of Hepatocellular Carcinoma for Local-Regional Intraarterial Therapies
Animal models play a crucial role in developing and testing new therapies for hepatocellular carcinoma (HCC), providing preclinical evidence prior to exploring human safety and efficacy outcomes. Interventional radiologists must weigh the advantages and disadvantages of various animal models available when testing a new local-regional therapy.
In an article published in Radiology: Imaging Cancer, Vishnu M. Chandra, MD, University of Virginia Health Systems, Charlottesville, and colleagues present a review of the currently available animal models for testing local-regional therapies for HCC. The team also discusses the importance of considering animal genetics, tumor biology and molecular mechanisms when ultimately choosing an animal model.
According to the researchers, emphasis should be placed on choosing a model with a tumor and microenvironment that most closely resemble those of humans. In addition, experiments should have reliable reproducibility and be performed in both a time- and a cost-efficient manner. “One approach that can be considered is performing initial translational experiments in cheaper and smaller tumor models to establish efficacy and then performing a more focused experiment in larger animals, with tumors more genetically similar to human HCC,” the authors conclude.
To read the full article, go to RSNA.org/ImagingCancer. Follow the Radiology: Imaging Cancer editor on Twitter @RadIC_Editor for more insights and highlights from the current issue.

